Nerve pain has a distinctive personality. It can burn or sting, tingle or throb, show up as sudden electric shocks or a deep ache that makes walking feel odd and sleep elusive. Whether it stems from a pinched spinal nerve, diabetes, chemotherapy, shingles, or an old ankle sprain that irritated a sensory branch, the patterns vary, but the theme is consistent: nerves behave differently from muscles and joints, and they respond to care on a slightly different timeline.
I spend a good portion of clinic days sorting through nerve pain stories. A software engineer whose toes buzz at night, a gardener with sciatic nerve pain flaring after weeding, a retired nurse living with post‑surgical numbness and hypersensitivity. They each want the same thing, which is fair: what works, and how fast. Natural remedies for nerve pain relief can help. They rarely replace a medical plan entirely, but they often amplify it, and sometimes they allow a person to reduce reliance on medications that cause fogginess or mood changes. The key is matching the remedy to the mechanism and giving nerves the resources and time they need to heal.
How nerve pain works, and why it lingers
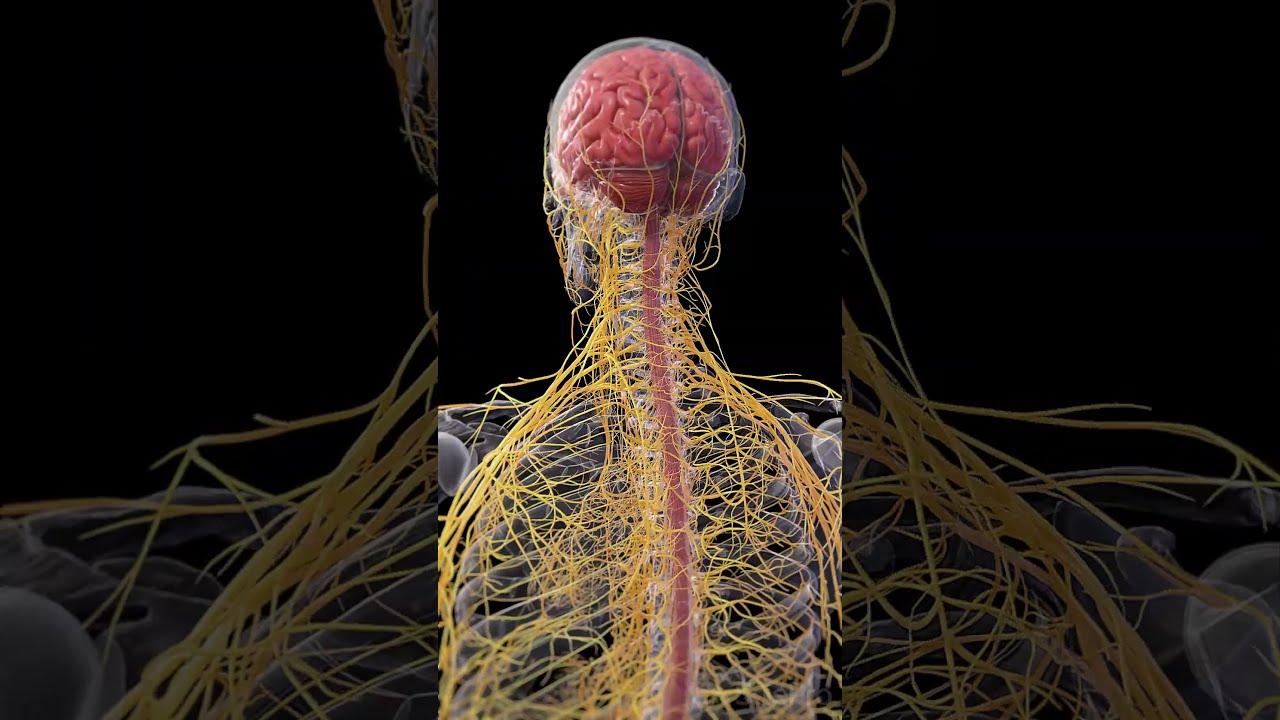
Nerves carry electrical signals with the help of insulating myelin, blood supply, and the supporting scaffolding of Schwann cells. Injury can damage any of these parts. Diabetic neuropathy usually involves metabolic stress on the small fibers. A herniated disc can inflame the root of a spinal nerve. Chemotherapy can poison rapidly dividing support cells. Even when the initial injury passes, nerves can stay irritable, like a smoke alarm that keeps chirping after the toast burns.
Healing happens, but it is slow. Peripheral nerves regenerate at roughly 1 to 5 millimeters per day under good conditions. That means a foot nerve damaged at the ankle might need several months. Spinal nerves compressed at the back can take even longer to settle because roots live in a tighter space and inflammation can recur with activity. Central nervous system injuries, such as spinal cord or brain lesions, are different and regenerate poorly, which is why identifying the injury type matters when asking can damaged nerves regenerate.
Signs of nerve healing after damage are often subtle: tingling that shifts from constant to intermittent, pins and needles that give way to duller sensations, or patches of returning light touch. Muscle strength may improve first, or sensation may lead. I usually ask people to track three markers weekly, not daily, because nerves fluctuate: pain intensity, footprint size (how large the symptomatic area feels), and function (sleep, walking, buttoning a shirt). Movement in any metric is encouraging.
When to see a clinician first
Natural strategies work best when the diagnosis is accurate. Early symptoms of nerve damage that deserve prompt evaluation include new foot drop, bowel or bladder changes, saddle numbness, severe weakness, rapidly climbing numbness, or nerve pain combined with fever or weight loss. A new case of numbness and tingling after starting a medication, chemotherapy, or an intense infection should also get medical review. Certain medications for neuropathic pain can be life‑changing and are worth discussing, even if your goal is treating nerve pain without opioids.
The nutrition foundation: vitamins for nerve repair and growth
Nerves are hungry tissue. The best diet for nerve healing emphasizes steady blood sugar, antioxidants, healthy fats, and adequate protein. For people with diabetic neuropathy, diabetic nerve pain natural treatment starts with glucose control, because high sugar levels reduce microvascular flow to nerves and create advanced glycation products that stiffen support tissues. Even modest improvements in A1c, for example from 8.5 to 7.5, can reduce progression and enhance the effect of therapies.
Several vitamins and cofactors serve as nerve repair supplements that work when deficiencies exist or when demand is high:
- B12 and methylation support: B12 deficiency can cause numbness, balance problems, and memory symptoms. Methylcobalamin is the form studied most for neuropathy. If serum B12 is borderline, methylmalonic acid and homocysteine clarify functional deficiency. Typical oral dosing ranges from 1,000 to 2,000 micrograms daily for several months. Vegans, older adults, patients on metformin or acid blockers, and those post‑bariatric surgery are higher risk. B1 and B6: Thiamine (B1) supports nerve conduction. Benfotiamine, a fat‑soluble derivative, has evidence in diabetic neuropathy at 300 to 600 mg daily. B6 helps, but high doses over time can paradoxically cause neuropathy. I keep B6 under 50 mg per day unless supervised. Alpha‑lipoic acid: An antioxidant that recycles glutathione and improves nerve blood flow. Evidence in diabetic neuropathy shows reduced burning and improved function at 600 mg daily, often noticeable after 3 to 8 weeks. It can lower blood sugar slightly, so diabetics should monitor. Acetyl‑L‑carnitine: Supports mitochondrial energy in nerves. Trials in chemotherapy‑induced and diabetic neuropathy used 500 to 1,000 mg two to three times daily for several months. Some people report improved numbness and vibration sense. Vitamin D and magnesium: Low vitamin D correlates with neuropathic pain severity. Repletion to mid‑normal ranges (often 2,000 to 4,000 IU daily, guided by labs) helps mood and pain thresholds. Magnesium glycinate or taurate, 200 to 400 mg nightly, can calm overactive nerves and improve sleep.
I do not stack every supplement at once. Start with two or three, give them 6 to 8 weeks, and watch for changes. People on chemotherapy, anticoagulants, or multiple medications should clear supplements with their oncologist or pharmacist.
Foods that help nerve regeneration, and a few to limit
Daily meals beat pills for long‑term nerve health. Omega‑3 fats from fish, flax, or algae supply DHA and EPA for myelin repair. Brightly colored plants, berries, leafy greens, and spices like turmeric and ginger add polyphenols that act as natural anti‑inflammatories for nerve pain. Beans, lentils, and eggs provide B vitamins and choline. Fermented foods can reduce systemic inflammation through the gut‑immune axis.
On the limiting side, high‑sugar drinks, excessive alcohol, and ultra‑processed snacks aggravate neuropathy. Alcohol directly injures nerves and depletes B vitamins. For some people, large loads of refined carbohydrates trigger next‑day flares, especially in nerve pain in feet treatment plans. If coffee worsens symptoms at night, shift the last cup to before noon.
Herbal remedies for nerve pain with real‑world traction
Herbs rarely mute severe neuropathic pain by themselves, but they can reduce intensity and reactivity. Curcumin (from turmeric), standardized with piperine for absorption, often eases shooting pain and stiffness at 500 to 1,000 mg daily. Boswellia, at 300 to 500 mg twice daily, provides additional anti‑inflammatory support and is gentler on the stomach than NSAIDs for many patients. Devil’s claw and willow bark help musculoskeletal components that co‑travel with radicular pain.
For calming hyperexcitable nerves, I often use lemon balm, passionflower, or skullcap in evening teas for two weeks as a trial. They do not fix nerve damage, but better sleep reduces perceived pain. If you use sedating herbs and also take nerve pain medications with side effects like drowsiness or dizziness, start low and avoid mixing new agents on the same night.
CBD oil for nerve pain relief shows mixed study results but enough real‑world benefit to justify a trial, especially for allodynia and sleep. Start with 10 to 25 mg oral CBD in the evening, titrate every 3 to 4 nights, and watch for interactions if you take anticoagulants.
Topical treatments for nerve damage: put help where it hurts
Topicals deliver relief without systemic fog. Capsaicin cream desensitizes TRPV1 receptors; low‑strength versions can be used at home twice daily for several weeks. The first week often stings, then calms. A high‑dose 8 percent capsaicin patch is a clinic procedure and can provide months of relief for localized neuropathic pain. Lidocaine 4 percent patches or gels numb painful skin without sedation and are useful for post‑herpetic neuralgia or tender scar lines. Compounded creams, such as amitriptyline‑ketamine or baclofen‑gabapentin, can help focal pain, though access varies.
If you are hunting for the best nerve pain cream in a store aisle, scan for lidocaine, capsaicin, menthol, or salicylate as active agents. Menthol provides a cooling distraction that sometimes reduces the brain’s spotlight on the pain, especially at night.

Cold vs heat therapy for nerve pain
I treat temperature as a dial. Cold calms a hot, inflamed nerve root after an acute flare, like sciatic nerve pain treatment at home following yard work. Ten to fifteen minutes with a wrapped ice pack, then movement, then repeat later. Heat relaxes protective muscle spasm that clamps around a cranky nerve. For chronic neuropathy in feet, gentle warmth and a short foot massage before bed can reduce tingling and help you fall asleep. Alternating contrast soaks, warm then cool, can improve small‑fiber circulation.
Movement as medicine: can exercise improve nerve function
Movement feeds nerves. Blood flow improves, inflammation resolves, and the brain rewires how it interprets signals. For peripheral neuropathy, I favor frequent small doses over rare heroic sessions. Walking most days, light cycling, or water exercise can transform chronic nerve pain management by lowering overall pain sensitivity.
Exercises for nerve pain in legs depend on cause. For sciatica, nerve glides or “flossing” restore mobility of the nerve through tight tunnels. Do not force end ranges or chase pain. Instead, move into a mild pull, back off, and repeat five to ten times, once or twice daily. For foot neuropathy, calf raises, toe spreading, and balance drills on a firm surface rebuild stability, which reduces stumbles and secondary injuries.
Yoga poses for nerve pain work by lengthening protective muscles, improving posture, and calming the nervous system. Child’s pose with arms forward for lumbar decompression, supported bridge for gentle hip extension, and supine hamstring stretches with a strap are staples. Stay in neutral‑neck positions if you have cervical radiculopathy. Poses should never cause zapping or limb weakness. If they do, modify or stop.
Strength training matters as nerves recover. When a nerve begins to reinnervate a muscle, timely load encourages the new connection to strengthen. Start with bodyweight, slow tempo, and a focus on quality contractions rather than heavy sets.
Manual and energy‑based therapies: where they fit
Massage therapy for nerve pain helps surrounding tissues reduce guarding. A therapist skilled in gentle myofascial techniques can decrease pressure on entrapment sites at the piriformis, tarsal tunnel, or thoracic outlet. Deep pressure directly over an irritable nerve is counterproductive, but decompressing layers above and below eases symptoms. Self‑massage with a soft ball against a wall, not a rigid lacrosse ball, is often better tolerated.
Acupuncture for nerve damage recovery shows moderate evidence for neuropathic pain and is helpful in practice when given as a short series. I tend to schedule six to eight sessions over three to four weeks, then reassess. Infrared therapy for nerve damage, including low‑level laser and red‑near infrared light, aims to support mitochondrial function and microcirculation. Small trials and clinician experience suggest benefit in peripheral neuropathy, particularly for burning feet. A reasonable home approach is three to five sessions weekly for 6 to 8 weeks with an FDA‑registered device, keeping the skin a comfortable warmth.
Nerve pain relief devices like TENS units can gate pain signals through competing sensory input. They help some people fall asleep or tolerate walking longer. Aim electrodes around, not on, the most sensitive area and try different pulse patterns.
Sleep, stress, and the overactive nervous system
What helps nerve pain at night is as much about the nervous system’s volume knob as the nerve’s local injury. A cool, dark room, regular wake time, and a simple pre‑bed routine lower background sympathetic tone. Magnesium, glycine, and chamomile tea before bed can help some people. If feet are burning, elevate calves on a soft bolster, use a breathable blanket that does not press on toes, and consider a lidocaine patch in the evening.
Ways to calm overactive nerves during the day include slow nasal breathing with longer exhales, brief mindfulness breaks that shift attention out of the painful area, and paced exposure to activities you avoid. Pain neuroscience education, even 20 minutes of reading or a short video, can reduce catastrophizing, which measurably reduces pain intensity.
Over‑the‑counter and non‑opioid options
Treating nerve pain without opioids is the norm in my practice. Over‑the‑counter medicine for nerve pain is limited, because NSAIDs and acetaminophen target inflammatory and nociceptive pain more than neuropathic pain. Still, they can help mixed pain states, such as spinal nerve pain treatment where muscle and joint components play a role. I use short, targeted courses rather than daily chronic use, and I watch stomach, kidney, and blood pressure risks.
Medications for neuropathic pain prescribed by clinicians, such as gabapentin, pregabalin, duloxetine, and tricyclics, have known nerve pain medications side effects. Drowsiness and brain fog are common early, then often fade. Natural strategies can lower the required dose, though tapering should be slow. Treating nerve pain without opioids does not mean you must avoid prescription options. It means we stack safer layers first and use minimum effective doses.
Home strategies when sciatica or focal nerve irritation flares
At‑home sciatic nerve pain treatment has a rhythm: unload the irritated nerve root, keep gentle blood flow, and avoid end‑range bending and twisting during the hot phase. A firm, neutral‑spine rest position with knees supported, a brief walking loop every hour while awake, and short bouts of nerve‑safe mobility work better than long bedrest. Heat on tight glute muscles, cold on the spine, and a topical agent can take the edge off. Most acute flares improve within 2 to 6 weeks; if leg weakness, foot drop, or bladder symptoms appear, seek medical care.
Peripheral neuropathy: building a home program that sticks
Treatment for peripheral neuropathy overlaps with general strategies, but consistent routines make the difference. Foot checks to prevent skin breakdown, supportive footwear with wide toe boxes, and balance drills reduce falls. For numbness and tingling treatment, daily foot rolling with a soft ball, contrast baths, and a 10‑minute walk can transform blood flow. If you sit most of the day, set a timer for micro‑walks, because long static positions often worsen symptoms.
Holistic treatments for neuropathy wrap medical care, nutrition, movement, and stress in a plan you can live with. If you are reading nerve pain supplements reviews, remember two truths: individual responses vary widely, and quality matters. Choose brands that test for heavy metals and verify potency.
How to repair nerves after injury, and how long does it take for nerves to heal
For focal injuries, such as a cut nerve repaired surgically, rehab for nerve damage recovery revolves around position sense retraining, graded strength, and desensitization of hypersensitive skin. A hand therapist can turn months of frustration into steady progress with tricks like texture exposure and mirror therapy. Nerve conduction therapy, as in EMG and NCS testing, does not fix nerves but helps track recovery and inform decisions.
Nerve damage recovery time depends on distance to target, age, metabolic health, and whether the nerve is compressed, inflamed, or severed. Partial injuries recover faster than complete ones. Is nerve pain reversible? Often yes, when the cause is metabolic, compressive, or inflammatory and you address the root. Signs of permanent nerve damage include persistent anesthesia, muscle atrophy that does not improve over a year, and severe denervation on repeat electrodiagnostic testing, though exceptions exist.
Alternative therapies for nerve damage: what the evidence and experience say
Stem cell therapy for nerve repair and nerve regeneration breakthroughs make hopeful headlines. Most work remains in early trials or specific surgical settings, such as nerve gaps bridged with conduits and grafts. For everyday neuropathy, emerging research on nerve regeneration focuses on growth factors, immune modulation, and metabolic pathways, not magic bullets yet. Infrared light and electrical stimulation have the most practical outpatient traction.
Alternative medicine for nerve pain should meet two tests: reasonable safety and a plausible mechanism. Acupuncture, yoga, mindfulness, and nutrition pass both. Extreme detoxes, megadose B6, and unregulated stem cell infusions fail at least one.
Pain flares and quick relief: ways to stop nerve pain instantly, with realistic expectations
There is no instant off‑switch, but a three‑step sprint often helps: change position to unload the nerve, apply a fast‑acting topical or temperature therapy, and give the brain a competing input like TENS or slow focused breathing. For some, a menthol gel and a 10‑minute walk beat an extra tablet. For others, a lidocaine patch and a quiet room do the trick. Keep a small “flare kit” ready so you do not rummage when your leg is on fire.
Putting it together at home: a compact starter plan
- Morning: 10‑minute walk, gentle nerve glide sequence, breakfast with protein and fiber. Take core supplements such as B12 (if indicated) and alpha‑lipoic acid. Midday: Posture reset and two minutes of slow breathing. Short stroll after lunch to stabilize blood sugar. Late afternoon: Strength or yoga session focused on quality movement. Apply heat to tight muscles if needed. Evening: Magnesium and tea, topical lidocaine or capsaicin on target areas, foot care routine. Lights out at a consistent time. Weekly: One manual therapy or acupuncture session during the first month, then taper based on response.
A word on safety and edge cases
People with bleeding risks should avoid high‑dose fish oil or certain herbs without clearance. If you are pregnant, breastfeeding, undergoing cancer treatment, or living with kidney or liver disease, discuss supplements with your clinician. If your pain pattern changes abruptly, if you notice new weakness, or if your balance worsens, re‑evaluate Click to find out more rather than pushing through.
Post‑surgical nerve damage recovery follows rules set by the surgeon and therapist. Too much early stretch can harm a repair. On the other hand, avoiding all motion can create adhesions that trap the nerve. Ask about timelines for glide versus strengthening, and document sensations week to week.
Living with progress, not perfection
The people who do best are not the ones who find a single perfect remedy. They stack modest wins and give them time to add up. They tune diet to their body rather than following fads. They use medications when needed and taper thoughtfully. They pay attention to sleep and stress because the nervous system listens to those signals as closely as it listens to vitamins and exercises.
Nerve healing is measured in millimeters per day and habits per week. If you nourish the system, move it kindly, and give it a calm place to work, it often rewards you with more comfortable feet, steadier hands, and quieter nights. And when you hit a plateau, that is the moment to reassess: adjust the plan, refresh the tools, or bring in a specialist who sees the patterns from a different angle.
Quick comparisons to help you choose
- For burning feet and diabetic neuropathy, alpha‑lipoic acid, glucose control, omega‑3s, and infrared light have a practical signal. Lidocaine patches help at night. For sciatica from a disc, position relief, gentle glides, short walks, anti‑inflammatory nutrition, and a limited course of NSAIDs can calm a flare. Massage the muscles, not the nerve. For post‑herpetic neuralgia, capsaicin or lidocaine topicals, gradual desensitization, and sleep optimization outperform frequent oral painkillers. For chemotherapy‑related neuropathy, coordinate with oncology. Acetyl‑L‑carnitine, gentle exercise, and acupuncture are considerations. Avoid supplements that conflict with your regimen. For mixed neck‑arm or low‑back‑leg patterns, combine posture, mobility, and targeted strengthening. A TENS unit can raise your activity ceiling.
Final perspective
You have many nerve pain treatment options that do not rely solely on pills. Natural remedies for nerve pain relief work best when anchored to clear goals, consistent routines, and honest feedback from your body. Not every supplement is worth your money, not every device lives up to its marketing, and not every day will be better than the last. Yet over months, a thoughtful mix of nutrition, movement, sleep care, topicals, and selective therapies can shift the trajectory. That is often the difference between enduring nerve pain and outgrowing it.